October is Breast Cancer Awareness Month
Breast Cancer-Associated Lymphedema
INCIDENCE AND RISK FACTORS
Breast cancer and its therapies are one of the most common causes of upper extremity lymphedema. In a systematic review that included 72 studies (29,612 women), the overall incidence of arm lymphedema in breast cancer survivors was 17 percent. The incidence varied based on the mode of diagnosis; it was 13, 15, and 20 percent based on clinical information, formal measurement (eg, arm circumference), and self-assessment, respectively.
Risk factors — The main risk factors for breast cancer-associated lymphedema (BCAL) include invasive cancer diagnosis, dissection/disruption of axillary lymph nodes, radiation therapy, local infection, and obesity, but other factors may also contribute.
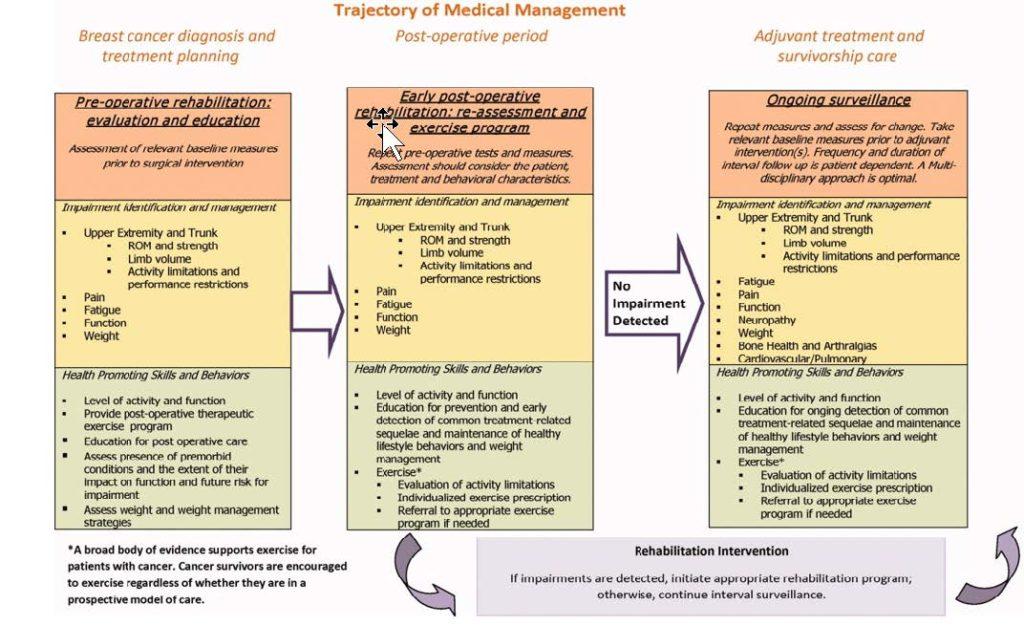
Early detection and intervention is key to managing the effects of lymphedema. Lymphedema (LE) must be diagnosed early. Often, LE is not diagnosed in its early stages when treatment is most effective. Referral to a Certified Lymphedema Therapist (CLT) at the earliest stage of treatment is essential to manage the disease before serious complications occur.
research hospitals.
5 https://www.lbbc.org/get-involved/breast-cancer-awarenessmonth#:~:text=October%20is%20Breast%20Cancer%20Awareness,people%20affected%20by%20breast%20cancer.
6 Author: Babak Mehrara, MDSection Editors:Daniel F Hayes, MDLarissa Nekhlyudov, MD, MPHEduardo Bruera, MDPatricia A Ganz, MDDeputy Editors:Kathryn A Collins, MD, PhD, FACSSadhna R Vora, MD
7 Cancer, Volume: 118, Issue: S8, Pages: 2191-2200, First published: 06 April 2012, DOI: (10.1002/cncr.27476)
October, Breast Cancer Awareness Month, is an annual campaign to raise awareness of this complex disease and fund research into causes, treatment, and cure. Since 1985, individuals, businesses, and communities have come together every October to show their support for the many people affected by breast cancer.
- In 2022, an estimated 290,560 new cases of invasive breast cancer are expected to be diagnosed in the U.S., along with 51,400 new cases of noninvasive breast cancer.
- An estimated 43,780 people will lose their lives to metastatic breast cancer.
- About 1 in 8 U.S. women and 1 in 833 U.S. men will develop invasive breast cancer over the course of their lives.
- As of 2020, there were 2.26 million global cases of breast cancer, making it the most commonly diagnosed cancer in the world. 685,000 of those diagnosed have died.1

September Recognizes Ovarian, Uterine, and Prostate Cancer Awareness

September brings a spotlight on ovarian, uterine and prostate cancers to broaden the conversation for meeting these unique needs. Lymphedema is often found in these patient populations. Lymphedema is a chronic, complex process that affects approximately 20 million people worldwide, causing significant discomfort, morbidity, and financial burden for those affected. Standardized methods for identifying at-risk patients and improved September Recognizes Ovarian, Uterine and Prostate Cancer Awareness The lowest rate of lower extremity lymphedema is found in ovarian cancer patients, ranging from 4.7% to 30.4% in prospective patient-reported surveys. The most important prognostic factor is Lymphadenectomy. The standard of care in ovarian cancer is surgical evaluation of the pelvic nodes and para-aortics up to the renal vessels for earlystage disease confined to the ovary and/or pelvis. Lim et al. examined a cohort of ovarian cancer patients with early-stage disease, 97.2% of whom underwent lymphadenectomy, and reported that 55% had lymphedema. It should be noted that 57.4% had greater than 35 lymph nodes excised. The majority of patients with newly diagnosed ovarian cancer actually present with advanced stage disease, in which case such a systematic lymphadenectomy is not routinely performed except in the setting of grossly enlarged nodes. 2 Ovarian Cancer provider education are greatly needed to address these issues. Newer, more objective measures, including patient-reported outcomes, can aid in the diagnosis and monitoring of treatment response. Prevention, early diagnosis, and timely interventions are key, but more research is needed to help us better understand lower extremity lymphedema. Patients who appear to be developing this condition should be referred in the early stages, when intervention has a greater chance of success. With risk mitigation, early diagnosis, and appropriate treatment, we can improve the quality of life for patients burdened by lower extremity lymphedema secondary to treatment of gynecologic malignancies.
Lymph from the gynecologic organs primarily drains into the three lymph node beds: pelvic, para-aortic, and inguinofemoral. These basins are often sampled or completely excised as part of the surgical management of gynecologic malignancies. According to this study, overall, the incidence of treatment-related lymphedema is about 25%, but it may be as high as 70% in some patient populations. There are two consistent contributors to lower extremity lymphedema in these patients: lymphadenectomy and radiation therapy. Lymphadenectomy— defined as complete excision of a lymph node basin—directly disrupts the normal return of lymphatic fluid from the lower extremities. In general, the risk of lymphedema is proportional to the number of lymph nodes sampled, with excision of certain lymph nodes and lymph node basins thought to present a higher risk. Sentinel lymph node mapping alone has been shown to decrease the risk of lower extremity lymphedema to less than 10%, across gynecologic malignancies. Radiation-induced lymphedema is thought to be secondary to lymph node and lymphatic vessel sclerosis, scarring, and subsequent impedance of upstream lymphatic flow. A systematic metaanalysis of all studies examining radiation and risk of lower extremity lymphedema in gynecologic cancer found the risk to be 34% in patients receiving radiation treatment. 1
Ovarian Cancer
The lowest rate of lower extremity lymphedema is found in ovarian cancer patients, ranging from 4.7% to 30.4% in prospective patient-reported surveys. The most important prognostic factor is Lymphadenectomy. The standard of care in ovarian cancer is surgical evaluation of the pelvic nodes and para-aortics up to the renal vessels for earlystage disease confined to the ovary and/or pelvis. Lim et al. examined a cohort of ovarian cancer patients with early-stage disease, 97.2% of whom underwent lymphadenectomy, and reported that 55% had lymphedema. It should be noted that 57.4% had greater than 35 lymph nodes excised. The majority of patients with newly diagnosed ovarian cancer actually present with advanced stage disease, in which case such a systematic lymphadenectomy is not routinely performed except in the setting of grossly enlarged nodes. 2
2 Lim MC, Lee JS, Nam BH, Seo SS, Kang S, Park SY. Lower extremity edema in patients with early ovarian cancer. J Ovarian Res 2014;7:28
Uterine Cancer
Uterine cancer includes endometrial cancer (more common) and uterine sarcoma. Uterine cancer symptoms include bleeding between periods or after menopause. Uterine cancer treatment often consists of a hysterectomy to remove the uterus (womb). Surgical lymphadenectomy and radiation are common components of therapy for women with endometrial cancer and are thought to increase the risk of developing lower-extremity lymphedema. These patients may also have conditions such as obesity that further increase their risk. “Once these conditions present, the symptoms and local effects of lymphedema can only be managed, not cured. The resulting disability may lead to severe lifelong morbidity including pain, skin breakdown, impaired mobility, difficulty with self-care, psychosocial morbidity, and impaired quality-of-life. The attributable risk of developing lower-extremity lymphedema was 23% for patients with endometrial cancer who underwent lymphadenectomy compared to hysterectomy alone, with an overall prevalence of 47%.” 3
3 Lymphedema After Surgery for Endometrial Cancer: Prevalence, Risk Factors, and Quality of Life Kathleen J. Yost, et al
Men and Lymphedema
Men are just as likely as women to develop lymphedema after surgery. There’s a stereotype that only women with breast cancer develop lymphedema, but that’s not true. The only cancer treatment that only men need to be concerned about is for prostate cancer. Lymphedema, which is swelling that happens when the body’s flow of lymph fluid is damaged or blocked, can occur following any surgery that removes or blocks lymph nodes or following radiation that can damage the superficial lymphatics. So, any cancer-related treatment that removes of blocks lymph nodes can cause lymphedema.
Risk Factors for Lymphedema
Risk factors depend on the type of surgery as well as the person’s individual risk factors. Statistics show approximately 16% of melanoma patients develop lymphedema, and approximately 10% of patients with cancers of the urinary system and/or genitals will experience lymphedema.
Someone’s individual risk factors may lead to development of lymphedema. These can include:
- Complexity of the surgery
- Whether the patient had radiation treatment
- The extent at which the lymph nodes were targeted
- If there was infection delaying the wound heal
- Whether the tumor was obstructing the lymph system prior to surgery
- If there was scarring from the surgery – scar tissue can act as a barrier to the lymph system
- Pre-existing condition such as diabetes, thyroid disease or obesity
- Stress
- People with venous disease in their legs prior to inguinal (groin area) lymph node removal4
4 Katherine Konosky, OTR/L, MS, CLT-LANA, Occupational Therapy


Ribbons participates in Tri-Cities Relay for Life
In 1985, Dr. Gordon “Gordy” Klatt started the first Relay For Life event in Tacoma, Washington. He endured 24 hours circling the track at the University of Puget Sound and raised $27,000 through pledges to help save lives from cancer. Since then, the Relay For Life movement has grown to more than 3,000 events in 29 countries across the globe. In 2021, Relay events in the US raised $60 million to help the American Cancer Society fight cancer. Ribbons Physical Therapy chose to participate in this year’s combined regional event held at East Tennessee State University to show its support of cancer survivors and caregivers in the community and provided free balance screenings to those who may continue to be suffering from peripheral neuropathy, one of the effects of chemotherapy treatment. To learn more about Relay For Life Tri-Cities go to https://tinyurl.com/y8xxdw2b.
How can we help your patients?
- Call to schedule an in-service to help identify patients with the potential for developing lymphedema who need to be screened or treated by our Certified Lymphedema Therapists
- Refer patients to our lymphedema monitoring program starting pre-procedure to establish baseline assessment and measurements, followed up one month after surgery/treatment, then quarterly for a year
- Do you want our lymphedema or cancer rehabilitation rack cards in your clinic to help patients understand why you are recommending us for treatment?
- If you have navigators, do you want patient handouts explaining our monitoring program and why you’re sending them to us?
Give us a call (423) 251-4742 or office@ribbonspt.com
If you desire to receive this newsletter electronically, please let us know:
Email: office@ribbonspt.com




